If You’ve Ever Had Pain After A UTI Is Gone, This Article Is For You.
by The Candidly Team
We used to think of UTIs primarily as an unfortunate side effect of sex. And that that can certainly be the case, especially amongst younger women.
But as we sail into our 40s and beyond, other factors come into play. According to Harvard Health, once we reach midlife “the main culprits behind recurrent UTIs are physical changes, including thinning of vaginal tissue, pelvic organ prolapse, incontinence, and trouble completely emptying the bladder. The lower levels of estrogen after menopause are also a factor.”
As women, about half of us will experience the hellishness of a UTI at least once in our lifetime. And sadly, there are times when that UTI won’t be knocked out with a round of antibiotics never to be heard from again. In fact, it’s estimated that about 77% of UTIs are relapsing infections. And many of those can include extended feelings of urgency, pelvic pain, back pain, and just feeling generally bad, long after the antibiotics have seemingly knocked out the infection.
Our point in stating all this is not to be all doom and gloom but to get you the answers we ourselves so craved about how to face the rocky path involved in dealing with a more “complicated” UTI.
And to deliver you those answers, we called upon the expertise of urologist Jill Peters-Gee, M.D., who wrote the book IC Journey to Wellness on healing bladder pain syndrome. She helped us break down what we need to know about what causes our most intrusive UTIs and more importantly, how we can help avoid them in the first place.
1) We all know what a UTI is, but what is a “complicated” UTI and how is it usually treated?
“A complicated’ UTI is an infection that has a higher chance of failing antibiotic therapy or a risk of adverse outcomes, i.e. spreading to the kidneys, blood, etc,” according to Peters-Gee.
This can be due to a series of factors that include:
Anatomical issues: such as “prolapse, obstruction, indwelling catheter, or a stone or foreign object being present.”
Functional issues: such as “incomplete emptying, underlying neurologic disease, and being immunocompromised.”
UTIs are also considered complicated when they occur in men or people who are on steroids or chemotherapy, have HIV, are older or immunocompromised, or have metabolic or hormonal abnormalities such as diabetes or pregnancy.
“Finally, if you have a highly resistant bacteria or a yeast or fungal infection, we will consider that a complicated UTI,” said Peters-Gee. “If you fall into any of these categories, a different approach is taken when treating. These infections typically require longer courses of treatment, different antibiotics, and sometimes, additional workups.”
2) Why are some doctors so befuddled when it comes to treating more complex UTIs?
“Most primary care physicians treat simple UTIs. Simple UTIs in non-pregnant women have been estimated to occur with as high as 0.7 infections per person per year. 50% of females with have at least one UTI at some point. Once they fail the standard therapy, then they are ‘complicated’ and will tend to get referred to a specialist for further treatment and workup. Unfortunately, with increasing antibiotic resistance, treatment failures are on the rise,” said Peters-Gee.
Image from Instagram / @Uqora
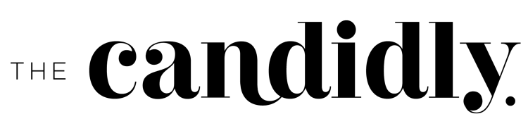
3) We’re starting to look into something called our “biofilm” (something else the doctors we’ve spoken with aren’t familiar with as it pertains to persistent or recurring UTIs). Is this an important thing to know about and why?
“We have typically thought of the biofilm, which is an encapsulated, structured microorganism colony, as something that attaches to catheters, stones, etc. A biofilm can also adhere to the bladder wall. When bacteria live in the biofilm, antibiotics cannot effectively penetrate it, and thus, often fail to eradicate the bacteria,” said Peters-Gee.
“Another concept that is emerging is that of our microbiome … Research on the microbiome has shown that we have “good” bacteria in the urine, that may have a protective effect. Alterations to this microbiome may contribute to infections as we enter menopause etc. Ongoing research will help us to understand this better.”
4) What is interstitial cystitis and how is it related to all of this?
“Interstitial Cystitis (IC) or Bladder Pain Syndrome ( BPS) is a diagnosis made when you have at least six weeks of symptoms, primarily pain, pressure, or discomfort, felt to be related to the bladder,” said Peters-Gee. “There are often other lower urinary tract symptoms such as frequent urination or urgency present as well. It is a diagnosis of exclusion, which means you must rule out infection or other pathology that could be causing the symptoms.”
“We still do not know what causes IC/BPS. There has never been a specific bacteria found that causes it. Research has shown us that there are different subtypes or phenotypes, which explains why different therapies work for different people. This is the focus of my book, IC Journey to Wellness. I provide ‘clues’ to help solve the mystery of what phenotype(s) are present. This then can be used to guide therapy, rather than the trial and error approach typically used,” said Peters-Gee.
5) The post-UTI pain can be truly unbearable. What’s happening to cause it and what can we do about it?
“When you have a UTI, the lining of the bladder becomes inflamed and, at times, can even bleed,” according to Peters-Gee. “When we look inside the bladder with a telescope (cystoscopy), it looks red, raw, and like someone has poked you in the eye 100 times! Even after the infection is gone, you can have symptoms of frequency, urgency, and sensitivity or pain.”
When it comes to what to do about it, Peters-Gee suggests:
Drink plenty of water, to keep the urine dilute, as a dilute urine is less irritating than a concentrated urine. “I always have told my patients ‘dilution is the solution to pollution!’ Water is your best friend as your bladder heals.”
Avoid dietary irritants, i.e. spicy foods, acidic foods, excessive caffeine, alcohol, artificial sweeteners.
“It can take up to six weeks in my experience for the bladder to look normal again,” said Peters-Gee. “Unfortunately, some women will get another UTI in this time because the inflamed bladder is like Velcro to bacteria, and it is easier for bacteria to stick to the surface.”
6) Are you a fan of Uqora? Do you recommend any other products or supplements?
“I have had many patients do well with Uqora,” said Peters-Gee. “Our bodies naturally make a small protein that goes to the bladder and floats around like a small dust particle. Its purpose is to bind to bacteria that might get into the bladder through the short urethra. Think sex, swimming pools, bubble baths, etc. The next time you urinate, the bacteria rinse out and don’t stick to the bladder lining. Uqora has three products. It uses D-Mannose to help bind to the bacteria and prevent adherence. There is also a biofilm buster of sorts, and a women’s health probiotic. Anytime you take antibiotics, you can kill off the good bacteria in the vagina. The probiotic may help to restore the good vaginal flora, which in theory, will help prevent the vicious cycle of vaginitis or another UTI.”
7) What are some foods we should eat OR stay away from if we’re managing complicated UTIs or interstitial cystitis?
Drink water: “The key thing with complicated UTIs is hydration.”
Empty your bladder all the way: “A simple trick is to sit comfortably and relax. Imagine your pelvic floor dropping down (opposite of a kegel). Then pretend you are blowing out a birthday candle slowly.”
Eat foods rich in both prebiotics and probiotics: “When you have recurrent UTIs or have taken antibiotics, it is important to restore your normal flora. Think good bacteria, like yogurt, kombucha, fermented foods.”
Limit sugar: “It is important for diabetics to have good glycemic control. Sugar or glucose in the urine is food for bacteria.”
Get to know your sensitivities: “Not all IC patients are sensitive to diet. The list is different for everyone. In general, acid foods, spicy foods, highly processed foods with a lot of additives are a no. Caffeine, artificial sweeteners, alcohol, chocolate, citrus tend to be aggravating, but not for everyone.”
8) Sooooo, no coffee? How do we live? Can we take a caffeine pill or does this still affect us the same way as coffee?
“If caffeine is an irritant, then sometimes it is the acid that really bothers you.” said Peters-Gee. “You can try Prelief, an OTC buffer that alkalinizes the urine. There are also low acid coffees available, coffee made from chicory, and Teeccino coffee and tea that sensitive bladders can tolerate.”
9) Any other helpful things we must know that we didn’t ask about? Tell us every little detail.
“Menopause or low estrogen (which can happen with OCP as well) can increase your risk of getting UTIs,” said Peters-Gee. “Low estrogen changes the vaginal pH, which then leads to a change in the vaginal flora. Thinning of the vaginal tissues can lead to pain with sex, itching, and dryness. There are many ways to address this. Topical estrogen and non-estrogen products like hyaluronic acid suppositories (Revaree is a good example) can help prevent recurrent UTIs.”
“I have had a lot of women start getting recurrent UTI’s with Peloton riding. Best advice is to treat your workout like sex. Urinate afterwards. We have very short urethras, and it is only a hop, skip, and a jump for bacteria to get up into the bladder. Hydrate and rinse those devils out. Void when you get out of the pool, off the bike, etc. And remember, ‘dilution is the solution to pollution!’
And to arm you with your own toolkit to help prevent a UTI:
Talk to your doctor: First and foremost. It’s the only way to truly decode what’s going on in your particular body.
Drink tons of water. We know. It’s hard. Here’s how we hack it.
Eat a balanced diet: Including those pre and probiotics we talked about.
Avoid eating irritating foods: spicy, acidic, caffeine, alcohol, artificial sweeteners, excess sugar, processed foods
Take extra time to pee: Really wait until your bladder is empty, even pausing for a beat, and trying again before you’re on your way.
Follow THIS no-BS Guide to helping prevent UTIs
This article is for informational purposes only. It is not intended to be used in place of professional advice, medical treatment, or professional care in any way. This article is not intended to be and should not be a substitute for professional care, advice or treatment. Please consult with your physician or healthcare provider before changing any health regimen. This article is not intended to diagnose, treat, or prevent disease of any kind. Read our Terms & Conditions and Privacy Policy.